New insights into the mechanisms of epithelial–mesenchymal transition and implications for cancer
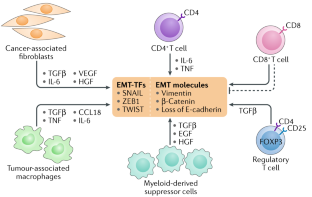
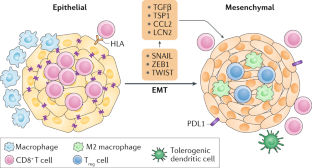
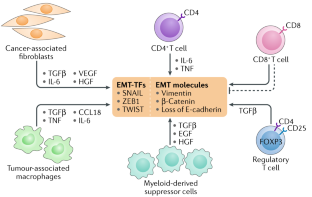
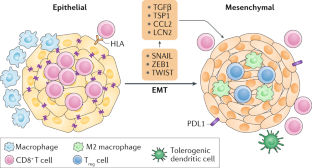
Epithelial–mesenchymal transition (EMT) is a cellular programme that is known to be crucial for embryogenesis, wound healing and malignant progression. During EMT, cell–cell and cell–extracellular matrix interactions are remodelled, which leads to the detachment of epithelial cells from each other and the underlying basement membrane, and a new transcriptional programme is activated to promote the mesenchymal fate. In the context of neoplasias, EMT confers on cancer cells increased tumour-initiating and metastatic potential and a greater resistance to elimination by several therapeutic regimens. In this Review, we discuss recent findings on the mechanisms and roles of EMT in normal and neoplastic tissues, and the cell-intrinsic signals that sustain expression of this programme. We also highlight how EMT gives rise to a variety of intermediate cell states between the epithelial and the mesenchymal state, which could function as cancer stem cells. In addition, we describe the contributions of the tumour microenvironment in inducing EMT and the effects of EMT on the immunobiology of carcinomas.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
206,07 € per year
only 17,17 € per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others

Linking EMT programmes to normal and neoplastic epithelial stem cells
Article 05 February 2021

The epithelial–mesenchymal plasticity landscape: principles of design and mechanisms of regulation
Article 11 May 2023

Guidelines and definitions for research on epithelial–mesenchymal transition
Article Open access 16 April 2020
References
- Nieto, M. A. Epithelial–mesenchymal transitions in development and disease: old views and new perspectives. Int. J. Dev. Biol.53, 1541–1547 (2009). PubMedGoogle Scholar
- Nieto, M. A., Huang, R. Y., Jackson, R. A. & Thiery, J. P. EMT: 2016. Cell166, 21–45 (2016). ArticleCASPubMedGoogle Scholar
- Kalluri, R. & Weinberg, R. A. The basics of epithelial–mesenchymal transition. J. Clin. Invest.119, 1420–1428 (2009). CASPubMedPubMed CentralGoogle Scholar
- Thiery, J. P., Acloque, H., Huang, R. Y. & Nieto, M. A. Epithelial–mesenchymal transitions in development and disease. Cell139, 871–890 (2009). CASPubMedGoogle Scholar
- Ye, X. et al. Distinct EMT programs control normal mammary stem cells and tumour-initiating cells. Nature525, 256–260 (2015). CASPubMedPubMed CentralGoogle Scholar
- Rhim, A. D. et al. EMT and dissemination precede pancreatic tumor formation. Cell148, 349–361 (2012). CASPubMedPubMed CentralGoogle Scholar
- Krebs, A. M. et al. The EMT-activator Zeb1 is a key factor for cell plasticity and promotes metastasis in pancreatic cancer. Nat. Cell Biol.19, 518–529 (2017). CASPubMedGoogle Scholar
- Mani, S. A. et al. The epithelial–mesenchymal transition generates cells with properties of stem cells. Cell133, 704–715 (2008). CASPubMedPubMed CentralGoogle Scholar
- Singh, A. & Settleman, J. EMT, cancer stem cells and drug resistance: an emerging axis of evil in the war on cancer. Oncogene29, 4741–4751 (2010). CASPubMedPubMed CentralGoogle Scholar
- Morel, A. P. et al. Generation of breast cancer stem cells through epithelial-mesenchymal transition. PLOS ONE3, e2888 (2008). This study, together with reference 8, demonstrates that carcinoma cells that have undergone EMT exhibit properties of stem cells. PubMedPubMed CentralGoogle Scholar
- Tam, W. L. & Weinberg, R. A. The epigenetics of epithelial–mesenchymal plasticity in cancer. Nat. Med.19, 1438–1449 (2013). CASPubMedPubMed CentralGoogle Scholar
- Shibue, T. & Weinberg, R. A. EMT, CSCs, and drug resistance: the mechanistic link and clinical implications. Nat. Rev. Clin. Oncol.14, 611–629 (2017). PubMedPubMed CentralGoogle Scholar
- Lambert, A. W., Pattabiraman, D. R. & Weinberg, R. A. Emerging biological principles of metastasis. Cell168, 670–691 (2017). CASPubMedPubMed CentralGoogle Scholar
- Kalluri, R. EMT: when epithelial cells decide to become mesenchymal-like cells. J. Clin. Invest.119, 1417–1419 (2009). CASPubMedPubMed CentralGoogle Scholar
- Olumi, A. F. et al. Carcinoma-associated fibroblasts direct tumor progression of initiated human prostatic epithelium. Cancer Res.59, 5002–5011 (1999). CASPubMedGoogle Scholar
- Kojima, Y. et al. Autocrine TGF-beta and stromal cell-derived factor-1 (SDF-1) signaling drives the evolution of tumor-promoting mammary stromal myofibroblasts. Proc. Natl Acad. Sci. USA107, 20009–20014 (2010). CASPubMedPubMed CentralGoogle Scholar
- Quail, D. F. & Joyce, J. A. Microenvironmental regulation of tumor progression and metastasis. Nat. Med.19, 1423–1437 (2013). CASPubMedPubMed CentralGoogle Scholar
- Terry, S. et al. New insights into the role of EMT in tumor immune escape. Mol. Oncol.11, 824–846 (2017). PubMedPubMed CentralGoogle Scholar
- Dongre, A. et al. Epithelial-to-mesenchymal transition contributes to immunosuppression in breast carcinomas. Cancer Res.77, 3982–3989 (2017). CASPubMedPubMed CentralGoogle Scholar
- Lamouille, S., Xu, J. & Derynck, R. Molecular mechanisms of epithelial-mesenchymal transition. Nat. Rev. Mol. Cell Biol.15, 178–196 (2014). CASPubMedPubMed CentralGoogle Scholar
- Bierie, B. et al. Integrin-β4 identifies cancer stem cell-enriched populations of partially mesenchymal carcinoma cells. Proc. Natl Acad. Sci. USA114, E2337–E2346 (2017). CASPubMedPubMed CentralGoogle Scholar
- Grande, M. T. et al. Snail1-induced partial epithelial-to-mesenchymal transition drives renal fibrosis in mice and can be targeted to reverse established disease. Nat. Med.21, 989–997 (2015). CASPubMedGoogle Scholar
- Batlle, E. et al. The transcription factor snail is a repressor of E-cadherin gene expression in epithelial tumour cells. Nat. Cell Biol.2, 84–89 (2000). CASPubMedGoogle Scholar
- Cano, A. et al. The transcription factor snail controls epithelial-mesenchymal transitions by repressing E-cadherin expression. Nat. Cell Biol.2, 76–83 (2000). CASPubMedGoogle Scholar
- Herranz, N. et al. Polycomb complex 2 is required for E-cadherin repression by the Snail1 transcription factor. Mol. Cell. Biol.28, 4772–4781 (2008). CASPubMedPubMed CentralGoogle Scholar
- Sanchez-Tillo, E. et al. ZEB1 represses E-cadherin and induces an EMT by recruiting the SWI/SNF chromatin-remodeling protein BRG1. Oncogene29, 3490–3500 (2010). CASPubMedGoogle Scholar
- Yang, M. H. et al. Bmi1 is essential in Twist1-induced epithelial-mesenchymal transition. Nat. Cell Biol.12, 982–992 (2010). PubMedGoogle Scholar
- Aigner, K. et al. The transcription factor ZEB1 (deltaEF1) promotes tumour cell dedifferentiation by repressing master regulators of epithelial polarity. Oncogene26, 6979–6988 (2007). CASPubMedPubMed CentralGoogle Scholar
- Spaderna, S. et al. The transcriptional repressor ZEB1 promotes metastasis and loss of cell polarity in cancer. Cancer Res.68, 537–544 (2008). CASPubMedGoogle Scholar
- Miyoshi, A. et al. Snail and SIP1 increase cancer invasion by upregulating MMP family in hepatocellular carcinoma cells. Br. J. Cancer90, 1265–1273 (2004). CASPubMedPubMed CentralGoogle Scholar
- Miyoshi, A. et al. Snail accelerates cancer invasion by upregulating MMP expression and is associated with poor prognosis of hepatocellular carcinoma. Br. J. Cancer92, 252–258 (2005). CASPubMedPubMed CentralGoogle Scholar
- Greenburg, G. & Hay, E. D. Epithelia suspended in collagen gels can lose polarity and express characteristics of migrating mesenchymal cells. J. Cell Biol.95, 333–339 (1982). CASPubMedGoogle Scholar
- Nieto, M. A., Sargent, M. G., Wilkinson, D. G. & Cooke, J. Control of cell behavior during vertebrate development by Slug, a zinc finger gene. Science264, 835–839 (1994). CASPubMedGoogle Scholar
- Lim, J. & Thiery, J. P. Epithelial–mesenchymal transitions: insights from development. Development139, 3471–3486 (2012). CASPubMedGoogle Scholar
- Oda, H., Tsukita, S. & Takeichi, M. Dynamic behavior of the cadherin-based cell-cell adhesion system during Drosophila gastrulation. Dev. Biol.203, 435–450 (1998). CASPubMedGoogle Scholar
- Schafer, G., Narasimha, M., Vogelsang, E. & Leptin, M. Cadherin switching during the formation and differentiation of the Drosophila mesoderm – implications for epithelial-to-mesenchymal transitions. J. Cell Sci.127, 1511–1522 (2014). PubMedGoogle Scholar
- Simoes-Costa, M. & Bronner, M. E. Establishing neural crest identity: a gene regulatory recipe. Development142, 242–257 (2015). CASPubMedPubMed CentralGoogle Scholar
- Shoval, I., Ludwig, A. & Kalcheim, C. Antagonistic roles of full-length N-cadherin and its soluble BMP cleavage product in neural crest delamination. Development134, 491–501 (2007). CASPubMedGoogle Scholar
- Clay, M. R. & Halloran, M. C. Cadherin 6 promotes neural crest cell detachment via F-actin regulation and influences active Rho distribution during epithelial-to-mesenchymal transition. Development141, 2506–2515 (2014). CASPubMedPubMed CentralGoogle Scholar
- Barrallo-Gimeno, A. & Nieto, M. A. The Snail genes as inducers of cell movement and survival: implications in development and cancer. Development132, 3151–3161 (2005). CASPubMedGoogle Scholar
- Aybar, M. J., Nieto, M. A. & Mayor, R. Snail precedes slug in the genetic cascade required for the specification and migration of the Xenopus neural crest. Development130, 483–494 (2003). CASPubMedGoogle Scholar
- Martinez-Alvarez, C. et al. Snail family members and cell survival in physiological and pathological cleft palates. Dev. Biol.265, 207–218 (2004). CASPubMedGoogle Scholar
- Stone, R. C. et al. Epithelial–mesenchymal transition in tissue repair and fibrosis. Cell Tissue Res.365, 495–506 (2016). CASPubMedPubMed CentralGoogle Scholar
- Savagner, P. & Arnoux, V. Epithelio-mesenchymal transition and cutaneous wound healing [French]. Bull. Acad. Natl Med.193, 1981–1991; discussion 1992 (2009). CASPubMedGoogle Scholar
- Savagner, P. et al. Developmental transcription factor slug is required for effective re-epithelialization by adult keratinocytes. J. Cell. Physiol.202, 858–866 (2005). CASPubMedGoogle Scholar
- Baumgart, E. et al. Identification and prognostic significance of an epithelial–mesenchymal transition expression profile in human bladder tumors. Clin. Cancer Res.13, 1685–1694 (2007). CASPubMedGoogle Scholar
- Gravdal, K., Halvorsen, O. J., Haukaas, S. A. & Akslen, L. A. A switch from E-cadherin to N-cadherin expression indicates epithelial to mesenchymal transition and is of strong and independent importance for the progress of prostate cancer. Clin. Cancer Res.13, 7003–7011 (2007). CASPubMedGoogle Scholar
- Kahlert, C. et al. Overexpression of ZEB2 at the invasion front of colorectal cancer is an independent prognostic marker and regulates tumor invasion in vitro. Clin. Cancer Res.17, 7654–7663 (2011). CASPubMedGoogle Scholar
- Lee, T. K. et al. Twist overexpression correlates with hepatocellular carcinoma metastasis through induction of epithelial-mesenchymal transition. Clin. Cancer Res.12, 5369–5376 (2006). CASPubMedGoogle Scholar
- Mahmood, M. Q., Ward, C., Muller, H. K., Sohal, S. S. & Walters, E. H. Epithelial mesenchymal transition (EMT) and non-small cell lung cancer (NSCLC): a mutual association with airway disease. Med. Oncol.34, 45 (2017). PubMedGoogle Scholar
- Migita, T. et al. Epithelial-mesenchymal transition promotes SOX2 and NANOG expression in bladder cancer. Lab. Invest.97, 567–576 (2017). CASGoogle Scholar
- Prudkin, L. et al. Epithelial-to-mesenchymal transition in the development and progression of adenocarcinoma and squamous cell carcinoma of the lung. Mod. Pathol.22, 668–678 (2009). CASPubMedPubMed CentralGoogle Scholar
- Roth, B. et al. Employing an orthotopic model to study the role of epithelial-mesenchymal transition in bladder cancer metastasis. Oncotarget8, 34205–34222 (2017). PubMedGoogle Scholar
- Shioiri, M. et al. Slug expression is an independent prognostic parameter for poor survival in colorectal carcinoma patients. Br. J. Cancer94, 1816–1822 (2006). CASPubMedPubMed CentralGoogle Scholar
- Yan, X. et al. N-Cadherin, a novel prognostic biomarker, drives malignant progression of colorectal cancer. Mol. Med. Rep.12, 2999–3006 (2015). CASPubMedGoogle Scholar
- Zhou, Z. J. et al. HNRNPAB induces epithelial-mesenchymal transition and promotes metastasis of hepatocellular carcinoma by transcriptionally activating SNAIL. Cancer Res.74, 2750–2762 (2014). CASPubMedGoogle Scholar
- Zhu, M. et al. Decreased TIP30 promotes Snail-mediated epithelial–mesenchymal transition and tumor-initiating properties in hepatocellular carcinoma. Oncogene34, 1420–1431 (2015). CASPubMedGoogle Scholar
- Blanco, M. J. et al. Correlation of Snail expression with histological grade and lymph node status in breast carcinomas. Oncogene21, 3241–3246 (2002). CASPubMedGoogle Scholar
- Yang, J. et al. Twist, a master regulator of morphogenesis, plays an essential role in tumor metastasis. Cell117, 927–939 (2004). CASPubMedGoogle Scholar
- Moody, S. E. et al. The transcriptional repressor Snail promotes mammary tumor recurrence. Cancer Cell8, 197–209 (2005). CASPubMedGoogle Scholar
- Vogelstein, B. et al. Allelotype of colorectal carcinomas. Science244, 207–211 (1989). CASPubMedGoogle Scholar
- Guo, W. et al. Slug and Sox9 cooperatively determine the mammary stem cell state. Cell148, 1015–1028 (2012). CASPubMedPubMed CentralGoogle Scholar
- Fischer, K. R. et al. Epithelial-to-mesenchymal transition is not required for lung metastasis but contributes to chemoresistance. Nature527, 472–476 (2015). CASPubMedPubMed CentralGoogle Scholar
- Zheng, X. et al. Epithelial-to-mesenchymal transition is dispensable for metastasis but induces chemoresistance in pancreatic cancer. Nature527, 525–530 (2015). CASPubMedPubMed CentralGoogle Scholar
- Ye, X. et al. Upholding a role for EMT in breast cancer metastasis. Nature547, E1–E3 (2017). CASPubMedPubMed CentralGoogle Scholar
- Aiello, N. M. et al. Upholding a role for EMT in pancreatic cancer metastasis. Nature547, E7–E8 (2017). CASPubMedPubMed CentralGoogle Scholar
- Cheung, K. J. et al. Polyclonal breast cancer metastases arise from collective dissemination of keratin 14-expressing tumor cell clusters. Proc. Natl Acad. Sci. USA113, E854–E863 (2016). CASPubMedPubMed CentralGoogle Scholar
- Tsai, J. H., Donaher, J. L., Murphy, D. A., Chau, S. & Yang, J. Spatiotemporal regulation of epithelial–mesenchymal transition is essential for squamous cell carcinoma metastasis. Cancer Cell22, 725–736 (2012). CASPubMedPubMed CentralGoogle Scholar
- Ocana, O. H. et al. Metastatic colonization requires the repression of the epithelial–mesenchymal transition inducer Prrx1. Cancer Cell22, 709–724 (2012). CASPubMedGoogle Scholar
- Cheung, K. J. & Ewald, A. J. A collective route to metastasis: seeding by tumor cell clusters. Science352, 167–169 (2016). CASPubMedPubMed CentralGoogle Scholar
- Puram, S. V. et al. Single-cell transcriptomic analysis of primary and metastatic tumor ecosystems in head and neck cancer. Cell171, 1611–1624.e24 (2017). CASPubMedPubMed CentralGoogle Scholar
- Iwadate, Y. Epithelial–mesenchymal transition in glioblastoma progression. Oncol. Lett.11, 1615–1620 (2016). CASPubMedPubMed CentralGoogle Scholar
- Fidler, I. J., Gersten, D. M. & Hart, I. R. The biology of cancer invasion and metastasis. Adv. Cancer Res.28, 149–250 (1978). CASPubMedGoogle Scholar
- Obenauf, A. C. & Massague, J. Surviving at a distance: organ specific metastasis. Trends Cancer1, 76–91 (2015). PubMedPubMed CentralGoogle Scholar
- Dressler, G. R. The cellular basis of kidney development. Annu. Rev. Cell Dev. Biol.22, 509–529 (2006). CASPubMedGoogle Scholar
- Li, B., Zheng, Y. W., Sano, Y. & Taniguchi, H. Evidence for mesenchymal–epithelial transition associated with mouse hepatic stem cell differentiation. PLOS ONE6, e17092 (2011). CASPubMedPubMed CentralGoogle Scholar
- Pattabiraman, D. R. & Weinberg, R. A. Targeting the epithelial-to-mesenchymal transition: the case for differentiation-based therapy. Cold Spring Harb. Symp. Quant. Biol.81, 11–19 (2016). PubMedGoogle Scholar
- Schmidt, J. M. et al. Stem-cell-like properties and epithelial plasticity arise as stable traits after transient Twist1 activation. Cell Rep.10, 131–139 (2015). The studies reported in references 21, 68, 69 and 78 demonstrate that partially mesenchymal cells have stem-like abilities and can readily form metastases. CASPubMedGoogle Scholar
- Beerling, E. et al. Plasticity between epithelial and mesenchymal states unlinks EMT from metastasis-enhancing stem cell capacity. Cell Rep.14, 2281–2288 (2016). CASPubMedPubMed CentralGoogle Scholar
- Pattabiraman, D. R. et al. Activation of PKA leads to mesenchymal-to-epithelial transition and loss of tumor-initiating ability. Science351, aad3680 (2016). This study delineates molecular players that can reverse the EMT, leading to the loss of stem-like features of carcinoma cells. PubMedPubMed CentralGoogle Scholar
- Bierie, B. & Moses, H. L. TGF-β and cancer. Cytokine Growth Factor Rev.17, 29–40 (2006). CASPubMedGoogle Scholar
- Xu, J., Lamouille, S. & Derynck, R. TGF-beta-induced epithelial to mesenchymal transition. Cell Res.19, 156–172 (2009). CASPubMedGoogle Scholar
- Derynck, R., Muthusamy, B. P. & Saeteurn, K. Y. Signaling pathway cooperation in TGF-β-induced epithelial-mesenchymal transition. Curr. Opin. Cell Biol.31, 56–66 (2014). CASPubMedPubMed CentralGoogle Scholar
- Mercado-Pimentel, M. E. & Runyan, R. B. Multiple transforming growth factor-beta isoforms and receptors function during epithelial–mesenchymal cell transformation in the embryonic heart. Cells Tissues Organs185, 146–156 (2007). CASPubMedGoogle Scholar
- Nawshad, A., LaGamba, D. & Hay, E. D. Transforming growth factor beta (TGFbeta) signalling in palatal growth, apoptosis and epithelial mesenchymal transformation (EMT). Arch. Oral Biol.49, 675–689 (2004). CASPubMedGoogle Scholar
- Gressner, A. M., Weiskirchen, R., Breitkopf, K. & Dooley, S. Roles of TGF-beta in hepatic fibrosis. Front. Biosci.7, d793–d807 (2002). CASPubMedGoogle Scholar
- Willis, B. C. & Borok, Z. TGF-beta-induced EMT: mechanisms and implications for fibrotic lung disease. Am. J. Physiol. Lung Cell. Mol. Physiol.293, L525–L534 (2007). CASPubMedGoogle Scholar
- Ramachandran, A. et al. TGF-β uses a novel mode of receptor activation to phosphorylate SMAD1/5 and induce epithelial-to-mesenchymal transition. eLife7, e31756 (2018). PubMedPubMed CentralGoogle Scholar
- Dhasarathy, A., Phadke, D., Mav, D., Shah, R. R. & Wade, P. A. The transcription factors Snail and Slug activate the transforming growth factor-beta signaling pathway in breast cancer. PLOS ONE6, e26514 (2011). CASPubMedPubMed CentralGoogle Scholar
- Gudey, S. K., Sundar, R., Heldin, C. H., Bergh, A. & Landstrom, M. Pro-invasive properties of Snail1 are regulated by sumoylation in response to TGFbeta stimulation in cancer. Oncotarget8, 97703–97726 (2017). PubMedPubMed CentralGoogle Scholar
- Ye, X. & Weinberg, R. A. The SUMO guards for SNAIL. Oncotarget8, 97701–97702 (2017). PubMedPubMed CentralGoogle Scholar
- Du, D. et al. Smad3-mediated recruitment of the methyltransferase SETDB1/ESET controls Snail1 expression and epithelial-mesenchymal transition. EMBO Rep.19, 135–155 (2017). PubMedPubMed CentralGoogle Scholar
- Xu, L. et al. Histone deacetylase 6 inhibition counteracts the epithelial–mesenchymal transition of peritoneal mesothelial cells and prevents peritoneal fibrosis. Oncotarget8, 88730–88750 (2017). PubMedPubMed CentralGoogle Scholar
- Grelet, S. et al. A regulated PNUTS mRNA to lncRNA splice switch mediates EMT and tumour progression. Nat. Cell Biol.19, 1105–1115 (2017). CASPubMedPubMed CentralGoogle Scholar
- Gregory, P. A. et al. The miR-200 family and miR-205 regulate epithelial to mesenchymal transition by targeting ZEB1 and SIP1. Nat. Cell Biol.10, 593–601 (2008). CASPubMedGoogle Scholar
- Korpal, M. & Kang, Y. The emerging role of miR-200 family of microRNAs in epithelial-mesenchymal transition and cancer metastasis. RNA Biol.5, 115–119 (2008). CASPubMedGoogle Scholar
- Grelet, S., McShane, A., Geslain, R. & Howe, P. H. Pleiotropic roles of non-coding RNAs in TGF-β-mediated epithelial–mesenchymal transition and their functions in tumor progression. Cancers9, 75 (2017). PubMed CentralGoogle Scholar
- Richards, E. J. et al. Long non-coding RNAs (LncRNA) regulated by transforming growth factor (TGF) beta: lncRNA-hit-mediated TGFbeta-induced epithelial to mesenchymal transition in mammary epithelia. J. Biol. Chem.290, 6857–6867 (2015). CASPubMedPubMed CentralGoogle Scholar
- Schmitz, S. U., Grote, P. & Herrmann, B. G. Mechanisms of long noncoding RNA function in development and disease. Cell. Mol. Life Sci.73, 2491–2509 (2016). CASPubMedPubMed CentralGoogle Scholar
- Klaus, A. & Birchmeier, W. Wnt signalling and its impact on development and cancer. Nat. Rev. Cancer8, 387–398 (2008). CASPubMedGoogle Scholar
- Zhan, T., Rindtorff, N. & Boutros, M. Wnt signaling in cancer. Oncogene36, 1461–1473 (2017). CASPubMedGoogle Scholar
- Clevers, H. Wnt/beta-catenin signaling in development and disease. Cell127, 469–480 (2006). CASPubMedGoogle Scholar
- Savagner, P. Leaving the neighborhood: molecular mechanisms involved during epithelial–mesenchymal transition. Bioessays23, 912–923 (2001). CASPubMedGoogle Scholar
- Liu, P. et al. Requirement for Wnt3 in vertebrate axis formation. Nat. Genet.22, 361–365 (1999). CASPubMedGoogle Scholar
- Garcia-Castro, M. I., Marcelle, C. & Bronner-Fraser, M. Ectodermal Wnt function as a neural crest inducer. Science297, 848–851 (2002). CASPubMedGoogle Scholar
- Arwert, E. N., Hoste, E. & Watt, F. M. Epithelial stem cells, wound healing and cancer. Nat. Rev. Cancer12, 170–180 (2012). CASPubMedGoogle Scholar
- Gonzalez, D. M. & Medici, D. Signaling mechanisms of the epithelial-mesenchymal transition. Sci. Signal.7, re8 (2014). PubMedPubMed CentralGoogle Scholar
- Tammela, T. et al. A Wnt-producing niche drives proliferative potential and progression in lung adenocarcinoma. Nature545, 355–359 (2017). CASPubMedPubMed CentralGoogle Scholar
- de Sousa e Melo, F. et al. A distinct role for Lgr5 + stem cells in primary and metastatic colon cancer. Nature543, 676–680 (2017). PubMedGoogle Scholar
- Batlle, E. & Clevers, H. Cancer stem cells revisited. Nat. Med.23, 1124–1134 (2017). CASPubMedGoogle Scholar
- Balsamo, J., Arregui, C., Leung, T. & Lilien, J. The nonreceptor protein tyrosine phosphatase PTP1B binds to the cytoplasmic domain of N-cadherin and regulates the cadherin-actin linkage. J. Cell Biol.143, 523–532 (1998). CASPubMedPubMed CentralGoogle Scholar
- Wu, Y. et al. Expression of Wnt3 activates Wnt/beta-catenin pathway and promotes EMT-like phenotype in trastuzumab-resistant HER2-overexpressing breast cancer cells. Mol. Cancer Res.10, 1597–1606 (2012). CASPubMedPubMed CentralGoogle Scholar
- Anastas, J. N. & Moon, R. T. WNT signalling pathways as therapeutic targets in cancer. Nat. Rev. Cancer13, 11–26 (2013). CASPubMedGoogle Scholar
- Stemmer, V., de Craene, B., Berx, G. & Behrens, J. Snail promotes Wnt target gene expression and interacts with beta-catenin. Oncogene27, 5075–5080 (2008). This study demonstrates crosstalk between the WNT and the TGFβ pathways, two different signalling cascades that can activate the EMT. CASPubMedGoogle Scholar
- Gauger, K. J., Chenausky, K. L., Murray, M. E. & Schneider, S. S. SFRP1 reduction results in an increased sensitivity to TGF-beta signaling. BMC Cancer11, 59 (2011). CASPubMedPubMed CentralGoogle Scholar
- Tang, Y., Liu, Z., Zhao, L., Clemens, T. L. & Cao, X. Smad7 stabilizes beta-catenin binding to E-cadherin complex and promotes cell-cell adhesion. J. Biol. Chem.283, 23956–23963 (2008). CASPubMedPubMed CentralGoogle Scholar
- Hoover, L. L. & Kubalak, S. W. Holding their own: the noncanonical roles of Smad proteins. Sci. Signal.1, pe48 (2008). PubMedPubMed CentralGoogle Scholar
- Scheel, C. et al. Paracrine and autocrine signals induce and maintain mesenchymal and stem cell states in the breast. Cell145, 926–940 (2011). CASPubMedPubMed CentralGoogle Scholar
- Dissanayake, S. K. et al. The Wnt5A/protein kinase C pathway mediates motility in melanoma cells via the inhibition of metastasis suppressors and initiation of an epithelial to mesenchymal transition. J. Biol. Chem.282, 17259–17271 (2007). CASPubMedGoogle Scholar
- Liu, J. et al. Downregulation of miR-200a induces EMT phenotypes and CSC-like signatures through targeting the beta-catenin pathway in hepatic oval cells. PLOS ONE8, e79409 (2013). PubMedPubMed CentralGoogle Scholar
- Su, J. et al. MicroRNA-200a suppresses the Wnt/beta-catenin signaling pathway by interacting with beta-catenin. Int. J. Oncol.40, 1162–1170 (2012). CASPubMedGoogle Scholar
- Ma, F. et al. MiR-23a promotes TGF-beta1-induced EMT and tumor metastasis in breast cancer cells by directly targeting CDH1 and activating Wnt/beta-catenin signaling. Oncotarget8, 69538–69550 (2017). PubMedPubMed CentralGoogle Scholar
- Zhang, J. Q. et al. MicroRNA-300 promotes apoptosis and inhibits proliferation, migration, invasion and epithelial-mesenchymal transition via the Wnt/beta-catenin signaling pathway by targeting CUL4B in pancreatic cancer cells. J. Cell. Biochem.119, 1027–1040 (2018). CASPubMedGoogle Scholar
- Osborne, B. A. & Minter, L. M. Notch signalling during peripheral T cell activation and differentiation. Nat. Rev. Immunol.7, 64–75 (2007). CASPubMedGoogle Scholar
- Kopan, R. Notch: a membrane-bound transcription factor. J. Cell Sci.115, 1095–1097 (2002). CASPubMedGoogle Scholar
- Bray, S. J. Notch signalling in context. Nat. Rev. Mol. Cell Biol.17, 722–735 (2016). CASPubMedGoogle Scholar
- Timmerman, L. A. et al. Notch promotes epithelial-mesenchymal transition during cardiac development and oncogenic transformation. Genes Dev.18, 99–115 (2004). CASPubMedPubMed CentralGoogle Scholar
- Bao, B. et al. Notch-1 induces epithelial-mesenchymal transition consistent with cancer stem cell phenotype in pancreatic cancer cells. Cancer Lett.307, 26–36 (2011). CASPubMedPubMed CentralGoogle Scholar
- Yuan, X. et al. Notch signaling and EMT in non-small cell lung cancer: biological significance and therapeutic application. J. Hematol. Oncol.7, 87 (2014). PubMedPubMed CentralGoogle Scholar
- Tang, Y. & Cheng, Y. S. miR-34a inhibits pancreatic cancer progression through Snail1-mediated epithelial-mesenchymal transition and the Notch signaling pathway. Sci. Rep.7, 38232 (2017). CASPubMedPubMed CentralGoogle Scholar
- Natsuizaka, M. et al. Interplay between Notch1 and Notch3 promotes EMT and tumor initiation in squamous cell carcinoma. Nat. Commun.8, 1758 (2017). PubMedPubMed CentralGoogle Scholar
- Zhang, J. et al. NUMB negatively regulates the epithelial-mesenchymal transition of triple-negative breast cancer by antagonizing Notch signaling. Oncotarget7, 61036–61053 (2016). PubMedPubMed CentralGoogle Scholar
- Liu, L. et al. Notch3 is important for TGF-beta-induced epithelial–mesenchymal transition in non-small cell lung cancer bone metastasis by regulating ZEB-1. Cancer Gene Ther.21, 364–372 (2014). CASPubMedGoogle Scholar
- Xing, F. et al. Hypoxia-induced Jagged2 promotes breast cancer metastasis and self-renewal of cancer stem-like cells. Oncogene30, 4075–4086 (2011). CASPubMedPubMed CentralGoogle Scholar
- Saad, S., Stanners, S. R., Yong, R., Tang, O. & Pollock, C. A. Notch mediated epithelial to mesenchymal transformation is associated with increased expression of the Snail transcription factor. Int. J. Biochem. Cell Biol.42, 1115–1122 (2010). CASPubMedGoogle Scholar
- Fukusumi, T. et al. The NOTCH4-HEY1 pathway induces epithelial mesenchymal transition in head and neck squamous cell carcinoma. Clin. Cancer Res.24, 619–633 (2017). PubMedPubMed CentralGoogle Scholar
- Blokzijl, A. et al. Cross-talk between the Notch and TGF-beta signaling pathways mediated by interaction of the Notch intracellular domain with Smad3. J. Cell Biol.163, 723–728 (2003). This study delineates how the TGFβ pathway impinges on the NOTCH signalling pathway. CASPubMedPubMed CentralGoogle Scholar
- Zavadil, J., Cermak, L., Soto-Nieves, N. & Bottinger, E. P. Integration of TGF-beta/Smad and Jagged1/Notch signalling in epithelial-to-mesenchymal transition. EMBO J.23, 1155–1165 (2004). CASPubMedPubMed CentralGoogle Scholar
- Morrissey, J. et al. Transforming growth factor-beta induces renal epithelial jagged-1 expression in fibrotic disease. J. Am. Soc. Nephrol.13, 1499–1508 (2002). CASPubMedGoogle Scholar
- Di Domenico, M. & Giordano, A. Signal transduction growth factors: the effective governance of transcription and cellular adhesion in cancer invasion. Oncotarget8, 36869–36884 (2017). PubMedPubMed CentralGoogle Scholar
- Grotegut, S., von Schweinitz, D., Christofori, G. & Lehembre, F. Hepatocyte growth factor induces cell scattering through MAPK/Egr-1-mediated upregulation of Snail. EMBO J.25, 3534–3545 (2006). CASPubMedPubMed CentralGoogle Scholar
- Tashiro, E., Henmi, S., Odake, H., Ino, S. & Imoto, M. Involvement of the MEK/ERK pathway in EGF-induced E-cadherin down-regulation. Biochem. Biophys. Res. Commun.477, 801–806 (2016). CASPubMedGoogle Scholar
- Tian, Y. C. et al. Epidermal growth factor and transforming growth factor-beta1 enhance HK-2 cell migration through a synergistic increase of matrix metalloproteinase and sustained activation of ERK signaling pathway. Exp. Cell Res.313, 2367–2377 (2007). CASPubMedGoogle Scholar
- Uttamsingh, S. et al. Synergistic effect between EGF and TGF-beta1 in inducing oncogenic properties of intestinal epithelial cells. Oncogene27, 2626–2634 (2008). CASPubMedGoogle Scholar
- Lo, H. W. et al. Epidermal growth factor receptor cooperates with signal transducer and activator of transcription 3 to induce epithelial–mesenchymal transition in cancer cells via up-regulation of TWIST gene expression. Cancer Res.67, 9066–9076 (2007). CASPubMedPubMed CentralGoogle Scholar
- Colomiere, M. et al. Cross talk of signals between EGFR and IL-6R through JAK2/STAT3 mediate epithelial–mesenchymal transition in ovarian carcinomas. Br. J. Cancer100, 134–144 (2009). CASPubMedGoogle Scholar
- Kim, J., Kong, J., Chang, H., Kim, H. & Kim, A. EGF induces epithelial–mesenchymal transition through phospho-Smad2/3-Snail signaling pathway in breast cancer cells. Oncotarget7, 85021–85032 (2016). PubMedPubMed CentralGoogle Scholar
- Fukuda, S. et al. Reversible interconversion and maintenance of mammary epithelial cell characteristics by the ligand-regulated EGFR system. Sci. Rep.6, 20209 (2016). CASPubMedPubMed CentralGoogle Scholar
- Miyazono, K., Ehata, S. & Koinuma, D. Tumor-promoting functions of transforming growth factor-beta in progression of cancer. Ups. J. Med. Sci.117, 143–152 (2012). PubMedPubMed CentralGoogle Scholar
- Shirakihara, T. et al. TGF-beta regulates isoform switching of FGF receptors and epithelial–mesenchymal transition. EMBO J.30, 783–795 (2011). CASPubMedPubMed CentralGoogle Scholar
- Maehara, O. et al. Fibroblast growth factor-2-mediated FGFR/Erk signaling supports maintenance of cancer stem-like cells in esophageal squamous cell carcinoma. Carcinogenesis38, 1073–1083 (2017). CASPubMedPubMed CentralGoogle Scholar
- McNiel, E. A. & Tsichlis, P. N. Analyses of publicly available genomics resources define FGF-2-expressing bladder carcinomas as EMT-prone, proliferative tumors with low mutation rates and high expression of CTLA-4, PD-1 and PD-L1. Signal Transduct. Target. Ther.2, 16045 (2017). PubMedPubMed CentralGoogle Scholar
- Hu, Y., Feng, X., Mintz, A., Jeffrey Petty, W. & Hsu, W. Regulation of brachyury by fibroblast growth factor receptor 1 in lung cancer. Oncotarget7, 87124–87135 (2016). PubMedPubMed CentralGoogle Scholar
- Qi, L. et al. FGF4 induces epithelial–mesenchymal transition by inducing store-operated calcium entry in lung adenocarcinoma. Oncotarget7, 74015–74030 (2016). PubMedPubMed CentralGoogle Scholar
- Ogunwobi, O. O., Puszyk, W., Dong, H. J. & Liu, C. Epigenetic upregulation of HGF and c-Met drives metastasis in hepatocellular carcinoma. PLOS ONE8, e63765 (2013). CASPubMedPubMed CentralGoogle Scholar
- Canadas, I. et al. High circulating hepatocyte growth factor levels associate with epithelial to mesenchymal transition and poor outcome in small cell lung cancer patients. Oncotarget5, 5246–5256 (2014). PubMedPubMed CentralGoogle Scholar
- Sylvester, P. W. Targeting met mediated epithelial–mesenchymal transition in the treatment of breast cancer. Clin. Transl Med.3, 30 (2014). PubMedPubMed CentralGoogle Scholar
- Chen, Q. Y. et al. MiR-206 inhibits HGF-induced epithelial–mesenchymal transition and angiogenesis in non-small cell lung cancer via c-Met /PI3k/Akt/mTOR pathway. Oncotarget7, 18247–18261 (2016). PubMedPubMed CentralGoogle Scholar
- Li, Y. et al. MiR-182 inhibits the epithelial to mesenchymal transition and metastasis of lung cancer cells by targeting the Met gene. Mol. Carcinog.57, 125–136 (2018). CASPubMedGoogle Scholar
- Zhu, G. et al. PAK5-mediated E47 phosphorylation promotes epithelial–mesenchymal transition and metastasis of colon cancer. Oncogene35, 1943–1954 (2016). CASPubMedGoogle Scholar
- Tam, W. L. et al. Protein kinase C alpha is a central signaling node and therapeutic target for breast cancer stem cells. Cancer Cell24, 347–364 (2013). CASPubMedPubMed CentralGoogle Scholar
- Pistore, C. et al. DNA methylation variations are required for epithelial-to-mesenchymal transition induced by cancer-associated fibroblasts in prostate cancer cells. Oncogene36, 5551–5566 (2017). CASPubMedGoogle Scholar
- Shintani, Y. et al. IL-6 secreted from cancer-associated fibroblasts mediates chemoresistance in NSCLC by increasing epithelial–mesenchymal transition signaling. J. Thorac. Oncol.11, 1482–1492 (2016). PubMedGoogle Scholar
- Yu, Y. et al. Cancer-associated fibroblasts induce epithelial–mesenchymal transition of breast cancer cells through paracrine TGF-beta signalling. Br. J. Cancer110, 724–732 (2014). CASPubMedGoogle Scholar
- Zhao, L. et al. An integrated analysis identifies STAT4 as a key regulator of ovarian cancer metastasis. Oncogene36, 3384–3396 (2017). CASPubMedGoogle Scholar
- Soon, P. S. et al. Breast cancer-associated fibroblasts induce epithelial-to-mesenchymal transition in breast cancer cells. Endocr. Relat. Cancer20, 1–12 (2013). CASPubMedGoogle Scholar
- Hsu, H. C. et al. Stromal fibroblasts from the interface zone of triple negative breast carcinomas induced epithelial–mesenchymal transition and its inhibition by emodin. PLOS ONE12, e0164661 (2017). PubMedPubMed CentralGoogle Scholar
- Goebel, L. et al. CD4 + T cells potently induce epithelial–mesenchymal-transition in premalignant and malignant pancreatic ductal epithelial cells - novel implications of CD4 + T cells in pancreatic cancer development. Oncoimmunology4, e1000083 (2015). PubMedPubMed CentralGoogle Scholar
- Kmieciak, M., Knutson, K. L., Dumur, C. I. & Manjili, M. H. HER-2/neu antigen loss and relapse of mammary carcinoma are actively induced by T cell-mediated anti-tumor immune responses. Eur. J. Immunol.37, 675–685 (2007). CASPubMedPubMed CentralGoogle Scholar
- Santisteban, M. et al. Immune-induced epithelial to mesenchymal transition in vivo generates breast cancer stem cells. Cancer Res.69, 2887–2895 (2009). CASPubMedPubMed CentralGoogle Scholar
- Cohen, E. N. et al. Inflammation mediated metastasis: immune induced epithelial-to-mesenchymal transition in inflammatory breast cancer cells. PLOS ONE10, e0132710 (2015). PubMedPubMed CentralGoogle Scholar
- Chen, Q. et al. Growth-induced stress enhances epithelial–mesenchymal transition induced by IL-6 in clear cell renal cell carcinoma via the Akt/GSK-3beta/beta-catenin signaling pathway. Oncogenesis6, e375 (2017). CASPubMedPubMed CentralGoogle Scholar
- Bonde, A. K., Tischler, V., Kumar, S., Soltermann, A. & Schwendener, R. A. Intratumoral macrophages contribute to epithelial–mesenchymal transition in solid tumors. BMC Cancer12, 35 (2012). CASPubMedPubMed CentralGoogle Scholar
- Fan, Q. M. et al. Tumor-associated macrophages promote cancer stem cell-like properties via transforming growth factor-beta1-induced epithelial–mesenchymal transition in hepatocellular carcinoma. Cancer Lett.352, 160–168 (2014). CASPubMedGoogle Scholar
- Bates, R. C. & Mercurio, A. M. Tumor necrosis factor-alpha stimulates the epithelial-to-mesenchymal transition of human colonic organoids. Mol. Biol. Cell14, 1790–1800 (2003). CASPubMedPubMed CentralGoogle Scholar
- Lin, E. Y., Nguyen, A. V., Russell, R. G. & Pollard, J. W. Colony-stimulating factor 1 promotes progression of mammary tumors to malignancy. J. Exp. Med.193, 727–740 (2001). CASPubMedPubMed CentralGoogle Scholar
- Qian, B. Z. & Pollard, J. W. Macrophage diversity enhances tumor progression and metastasis. Cell141, 39–51 (2010). This study delineates the molecular mechanisms by which macrophages induce metastasis of carcinoma cells. CASPubMedPubMed CentralGoogle Scholar
- Su, S. et al. A positive feedback loop between mesenchymal-like cancer cells and macrophages is essential to breast cancer metastasis. Cancer Cell25, 605–620 (2014). PubMedGoogle Scholar
- Lu, H. et al. A breast cancer stem cell niche supported by juxtacrine signalling from monocytes and macrophages. Nat. Cell Biol.16, 1105–1117 (2014). CASPubMedPubMed CentralGoogle Scholar
- Che, D. et al. Macrophages induce EMT to promote invasion of lung cancer cells through the IL-6-mediated COX-2/PGE2/beta-catenin signalling pathway. Mol. Immunol.90, 197–210 (2017). CASPubMedGoogle Scholar
- Gabrilovich, D. I. & Nagaraj, S. Myeloid-derived suppressor cells as regulators of the immune system. Nat. Rev. Immunol.9, 162–174 (2009). CASPubMedPubMed CentralGoogle Scholar
- Sangaletti, S. et al. Mesenchymal transition of high-grade breast carcinomas depends on extracellular matrix control of myeloid suppressor cell activity. Cell Rep.17, 233–248 (2016). CASPubMedGoogle Scholar
- Toh, B. et al. Mesenchymal transition and dissemination of cancer cells is driven by myeloid-derived suppressor cells infiltrating the primary tumor. PLOS Biol.9, e1001162 (2011). CASPubMedPubMed CentralGoogle Scholar
- Ouzounova, M. et al. Monocytic and granulocytic myeloid derived suppressor cells differentially regulate spatiotemporal tumour plasticity during metastatic cascade. Nat. Commun.8, 14979 (2017). CASPubMedPubMed CentralGoogle Scholar
- Ruffell, B. et al. Leukocyte composition of human breast cancer. Proc. Natl Acad. Sci. USA109, 2796–2801 (2012). CASPubMedGoogle Scholar
- Kerkar, S. P. & Restifo, N. P. Cellular constituents of immune escape within the tumor microenvironment. Cancer Res.72, 3125–3130 (2012). CASPubMedPubMed CentralGoogle Scholar
- Gajewski, T. F., Schreiber, H. & Fu, Y. X. Innate and adaptive immune cells in the tumor microenvironment. Nat. Immunol.14, 1014–1022 (2013). CASPubMedPubMed CentralGoogle Scholar
- Kudo-Saito, C., Shirako, H., Takeuchi, T. & Kawakami, Y. Cancer metastasis is accelerated through immunosuppression during Snail-induced EMT of cancer cells. Cancer Cell15, 195–206 (2009). This study shows that activation of EMT can induce the formation of immunosuppressive cells in melanomas and alter their response to checkpoint blockade therapy. CASPubMedGoogle Scholar
- Akalay, I. et al. Epithelial-to-mesenchymal transition and autophagy induction in breast carcinoma promote escape from T cell-mediated lysis. Cancer Res.73, 2418–2427 (2013). CASPubMedGoogle Scholar
- Akalay, I. et al. EMT impairs breast carcinoma cell susceptibility to CTL-mediated lysis through autophagy induction. Autophagy9, 1104–1106 (2013). CASPubMedPubMed CentralGoogle Scholar
- Wrzesinski, S. H., Wan, Y. Y. & Flavell, R. A. Transforming growth factor-beta and the immune response: implications for anticancer therapy. Clin. Cancer Res.13, 5262–5270 (2007). CASPubMedGoogle Scholar
- Teicher, B. A. Transforming growth factor-beta and the immune response to malignant disease. Clin. Cancer Res.13, 6247–6251 (2007). CASPubMedGoogle Scholar
- Viel, S. et al. TGF-β inhibits the activation and functions of NK cells by repressing the mTOR pathway. Sci. Signal.9, ra19 (2016). PubMedGoogle Scholar
- Bellone, G., Aste-Amezaga, M., Trinchieri, G. & Rodeck, U. Regulation of NK cell functions by TGF-beta 1. J. Immunol.155, 1066–1073 (1995). CASPubMedGoogle Scholar
- Kudo-Saito, C., Shirako, H., Ohike, M., Tsukamoto, N. & Kawakami, Y. CCL2 is critical for immunosuppression to promote cancer metastasis. Clin. Exp. Metastasis30, 393–405 (2013). CASPubMedGoogle Scholar
- Hsu, D. S. et al. Acetylation of snail modulates the cytokinome of cancer cells to enhance the recruitment of macrophages. Cancer Cell26, 534–548 (2014). CASPubMedGoogle Scholar
- Lovisa, S. et al. Epithelial-to-mesenchymal transition induces cell cycle arrest and parenchymal damage in renal fibrosis. Nat. Med.21, 998–1009 (2015). CASPubMedPubMed CentralGoogle Scholar
- Blum, J. S., Wearsch, P. A. & Cresswell, P. Pathways of antigen processing. Annu. Rev. Immunol.31, 443–473 (2013). CASPubMedPubMed CentralGoogle Scholar
- Garcia-Lora, A., Algarra, I. & Garrido, F. MHC class I antigens, immune surveillance, and tumor immune escape. J. Cell. Physiol.195, 346–355 (2003). CASPubMedGoogle Scholar
- Fruci, D. et al. Major histocompatibility complex class i and tumour immuno-evasion: how to fool T cells and natural killer cells at one time. Curr. Oncol.19, 39–41 (2012). CASPubMedPubMed CentralGoogle Scholar
- Tripathi, S. C. et al. Immunoproteasome deficiency is a feature of non-small cell lung cancer with a mesenchymal phenotype and is associated with a poor outcome. Proc. Natl Acad. Sci. USA113, E1555–E1564 (2016). CASPubMedPubMed CentralGoogle Scholar
- Noman, M. Z. et al. The immune checkpoint ligand PD-L1 is upregulated in EMT-activated human breast cancer cells by a mechanism involving ZEB-1 and miR-200. Oncoimmunology6, e1263412 (2017). PubMedPubMed CentralGoogle Scholar
- Chen, L. et al. Metastasis is regulated via microRNA-200/ZEB1 axis control of tumour cell PD-L1 expression and intratumoral immunosuppression. Nat. Commun.5, 5241 (2014). CASPubMedGoogle Scholar
- Lou, Y. et al. Epithelial–mesenchymal transition is associated with a distinct tumor microenvironment including elevation of inflammatory signals and multiple immune checkpoints in lung adenocarcinoma. Clin. Cancer Res.22, 3630–3642 (2016). CASPubMedPubMed CentralGoogle Scholar
- Celia-Terrassa, T. et al. Epithelial–mesenchymal transition can suppress major attributes of human epithelial tumor-initiating cells. J. Clin. Invest.122, 1849–1868 (2012). CASPubMedPubMed CentralGoogle Scholar
- Chaffer, C. L. et al. Normal and neoplastic nonstem cells can spontaneously convert to a stem-like state. Proc. Natl Acad. Sci. USA108, 7950–7955 (2011). CASPubMedPubMed CentralGoogle Scholar
- Chaffer, C. L., San Juan, B. P., Lim, E. & Weinberg, R. A. EMT, cell plasticity and metastasis. Cancer Metastasis Rev.35, 645–654 (2016). PubMedGoogle Scholar
- Lim, S. et al. SNAI1-mediated epithelial–mesenchymal transition confers chemoresistance and cellular plasticity by regulating genes involved in cell death and stem cell maintenance. PLOS ONE8, e66558 (2013). CASPubMedPubMed CentralGoogle Scholar
- Kurrey, N. K. et al. Snail and slug mediate radioresistance and chemoresistance by antagonizing p53-mediated apoptosis and acquiring a stem-like phenotype in ovarian cancer cells. Stem Cells27, 2059–2068 (2009). CASPubMedGoogle Scholar
- Bharti, R., Dey, G. & Mandal, M. Cancer development, chemoresistance, epithelial to mesenchymal transition and stem cells: a snapshot of IL-6 mediated involvement. Cancer Lett.375, 51–61 (2016). CASPubMedGoogle Scholar
- Pattabiraman, D. R. & Weinberg, R. A. Tackling the cancer stem cells — what challenges do they pose? Nat. Rev. Drug Discov.13, 497–512 (2014). CASPubMedPubMed CentralGoogle Scholar
- Sullivan, N. J. et al. Interleukin-6 induces an epithelial–mesenchymal transition phenotype in human breast cancer cells. Oncogene28, 2940–2947 (2009). CASPubMedPubMed CentralGoogle Scholar
- Jurmeister, S. et al. MicroRNA-200c represses migration and invasion of breast cancer cells by targeting actin-regulatory proteins FHOD1 and PPM1F. Mol. Cell. Biol.32, 633–651 (2012). CASPubMedPubMed CentralGoogle Scholar
- Cochrane, D. R., Howe, E. N., Spoelstra, N. S. & Richer, J. K. Loss of miR-200c: a marker of aggressiveness and chemoresistance in female reproductive cancers. J. Oncol.2010, 821717 (2010). PubMedGoogle Scholar
- Fidler, I. J. Tumor heterogeneity and the biology of cancer invasion and metastasis. Cancer Res.38, 2651–2660 (1978). CASPubMedGoogle Scholar
Acknowledgements
The authors thank T. Shibue and A. W. Lambert for critical reading of the manuscript. The authors thank R. Lee for helping with preparation of the figures. A.D. was supported by a postdoctoral fellowship from the Ludwig Fund for Cancer Research. R.A.W. is an American Cancer Society research professor and a Daniel K. Ludwig Foundation cancer research professor. The work of the authors has been supported by grants from the US National Institutes of Health (NIH) (P01 CA080111), Breast Cancer Research Foundation, Samuel Waxman Cancer Research Foundation, Breast Cancer Alliance and the Ludwig Center for Molecular Oncology.